Largest study of nose microbiome helps highlight those at risk of Staph aureus infection
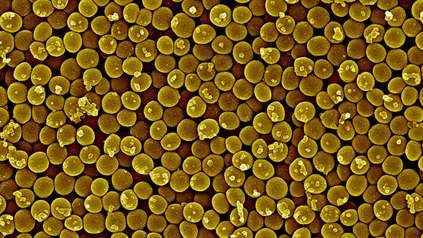
People who persistently carry Staphylococcus aureus (S. aureus) in their nose have fewer species of other bacteria, while certain bacteria may help to prevent S. aureus colonisation.
These are the findings of the largest-ever study of the nasal microbiome, published today (2 December) in Nature Communications.
In the study, researchers at the Wellcome Sanger Institute, University of Cambridge, the University of Birmingham, and Imperial College London analysed nasal swabs from over 1,000 healthy blood donors to explore the complex bacterial communities living in the human nose.
The research sheds new light on how interactions between different bacterial species are key to understanding why some people are persistently colonised by S. aureus and also provides clinical insight into predicting who may be most at risk of S. aureus infection.
S. aureus is a common bacterium that lives without symptoms in the nose of about 30 per cent of people.1 Normally it does not cause harm, but if it enters the body through wounds, cuts, or surgical incisions it can cause serious infections. Infections from S. aureus are the second most common cause of mortality related to bacterial infections, after tuberculosis, causing roughly one million deaths per year.2 Some strains, such as methicillin-resistant S. aureus (MRSA), are resistant to common antibiotics, making infections harder to treat.
Historically, carriers of S. aureus have been classified into three groups: persistent carriers, intermittent carriers, and non-carriers. Persistent carriers always test positive for carrying S. aureus. An intermittent carrier sometimes tests positive, and non-carriers never show positive for carrying S. aureus.
Because S. aureus carriage increases the risk of post-operative infections, hospitals often screen patients before procedures, such as joint replacements, and may provide nasal treatments to reduce colonisation. However, the nasal microbiome, unlike the gut microbiome, has not been studied in large populations, leaving much unknown about how S. aureus interacts with other nasal bacteria.
In a new study, researchers at the Sanger Institute and their collaborators sought to analyse a much larger group of people than in previous studies to thoroughly understand how different bacteria can influence S. aureus colonisation.
The study recruited volunteers from across England who had previously taken part in trials of blood donation led by the University of Cambridge.3,4 The team collected three weekly nasal swabs from 1,100 healthy adults.5,6 Each sample was tested for S. aureus using standard lab culture techniques and DNA sequencing was performed to identify the full range of bacterial species present in each nose swab. Researchers used advanced statistical methods to uncover patterns in the nasal microbiome and determine whether S. aureus carriage could be predicted by the bacterial community.
The researchers found two main patterns in the microbiome. Firstly, the team found that persistent carriers have a distinct microbiome with an abundance of S. aureus and a lack of other species in the nasal samples.
Secondly, certain bacteria such as Staphylococcus epidermidis, Dolosigranulum pigrum, and Moraxella catarrhalis were found to be less common in persistent carriers. The researchers suggest that these other species might help block S. aureus colonisation in non-carriers.
Using machine learning, the researchers were also able to predict who is persistently colonised with S. aureus particularly well, offering a possible method to predict risk of infection.
Interestingly, the researchers also propose that intermittent carriers are just misclassified persistent carriers or non-carriers — the notion of intermittent carriage does not represent a true biological state. They are likely to be non-carriers who have been exposed to and picked up S. aureus for a short period of time.
This study highlights that interactions between different bacterial species are key to understanding why some people are persistently colonised by S. aureus, placing them at greater risk of infection. The findings have important clinical implications. Identifying carriers of S. aureus could help predict infection risk and enable healthcare professionals to better target those who may benefit from preventive decolonisation treatments.
The researchers now want to build on this piece of the puzzle by looking into whether certain risk factors, such as medical conditions, sex, human genetics or other environmental exposures influence S. aureus carriage.
“Persistent Staphylococcus aureus carriage is a well-recognised risk factor for infection, particularly in hospital settings. By identifying the bacterial profiles that protect against S. aureus colonisation, our findings could inform new, microbiome-based strategies to reduce infection risk without relying on antibiotics.”
Dr Dinesh Aggarwal, first author and Clinical Lecturer at Imperial College London
“This is the largest study to date of the bacteria that live in our noses, and it shows that Staphylococcus aureus doesn’t act alone — it’s part of a whole community. We found that some bacterial neighbours can help keep Staph out, offering exciting new directions for preventing infections using new methods.”
Katie Bellis, co-author and Staff Scientist at the Wellcome Sanger Institute
“Everyone’s nose microbiome is unique, and this study shows that the bacteria living there can have a big impact on our health. By studying thousands of samples, we can finally see the bigger picture of how our natural bacteria either help or hinder infection.”
Dr Ewan Harrison, senior author and Group Leader at the Wellcome Sanger Institute and University of Cambridge
More information
Notes to Editors:
- Centers for Disease Control and Prevention (CDC). April 2024. Staphylococcus aureus Basics. [Last accessed: November 2025].
- GBD 2019 Antimicrobial Resistance Collaborators. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. DOI: 10.1016/S0140-6736(22)02185-7
- For more information on The National Institute for Health and Care Research (NIHR) Blood and Transplant Research Unit (BTRU) in Donor Health and Behaviour, please visit: BTRU Donor Health – Research on increasing blood donation and protecting the health of blood donors
- For more information on the CARRIAGE study, please visit: https://www.carriagestudy.org.uk/
- S. aureus colonisation status was defined as:
- Persistent carriers – S. aureus detected in all three swabs
- Intermittent carriers – S. aureus detected in one or two swabs
- Non-carriers – S. aureus not detected in any swab
- In this observational cohort study, nasal samples taken from the anterior nares were obtained from healthy human participants from the community participating in the CARRIAGE study between 13th October 2016 and 17th May 2017.
Publication
D. Aggarwal, K. Bellis, B. Blane et al. (2025) ‘Large-scale characterization of the nasal microbiome redefines Staphylococcus aureus colonization status’. Nature Communications. DOI: 10.1038/s41467-025-66564-4
Funding
This research was supported in part by a Wellcome Collaborative Award in Science as well as funding from the UK Research and Innovation (UKRI) and National Institute for Health and Care Research (NIHR). A full list of acknowledgements can be found in the publication.