Hidden evolution in sperm raises disease risk for children as men age
Harmful genetic changes in sperm become substantially more common as men age because some are actively favoured during sperm production, new research has revealed.
In a landmark study published today (8 October) in Nature, researchers from the Wellcome Sanger Institute, in collaboration with the TwinsUK study at King’s College London, have comprehensively mapped how harmful DNA changes in sperm cells can increase across the genome as men age.
The findings create new possibilities to explore how lifestyle and environmental factors might influence genetic risks passed on to future generations.
In renewing tissues, mutations – changes in DNA – can give cells a competitive advantage leading to ‘clones’ of cells that carry the same mutations. Groups of these clones then expand to outgrow other cells. Unlike mutations in ordinary, or somatic cells, which make up connective tissue, bones and organs, mutations in sperm and egg cells are transmitted to the next generation of offspring. However, until recently, it has been difficult to measure how strongly these mutations are favoured in sperm because DNA sequencing methods were not accurate enough.
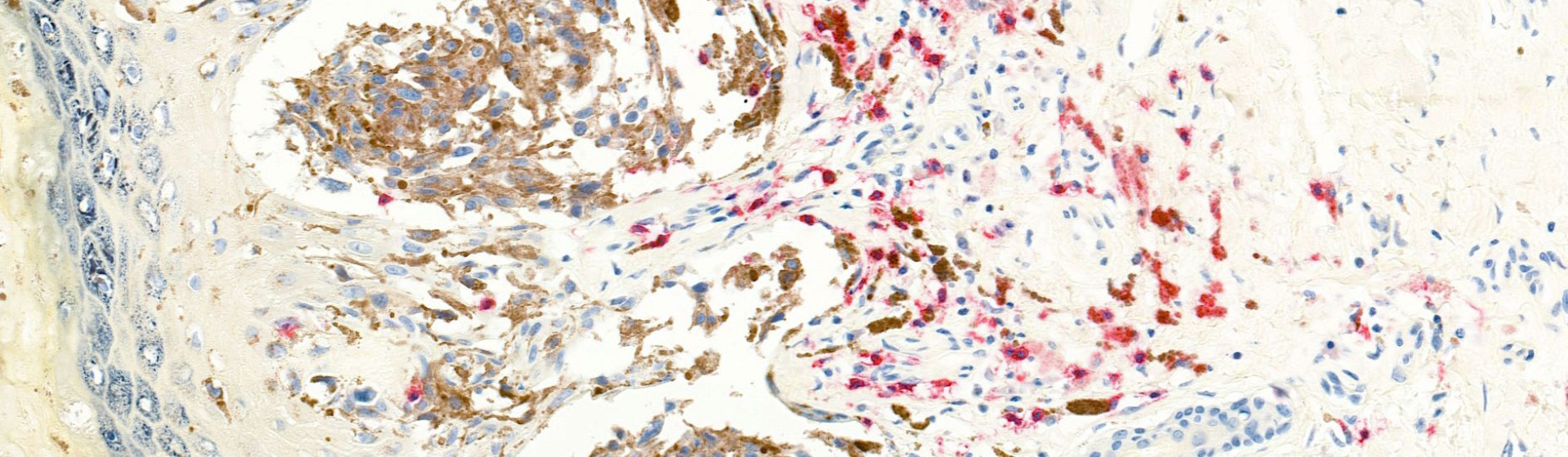
In a new study, researchers used NanoSeq,1 an ultra-accurate DNA sequencing method to analyse sperm from 81 healthy men, aged between 24 and 75 years, with unprecedented precision.2, 3 The sperm samples were collected as part of the TwinsUK cohort, the UK’s largest adult twin registry, providing a unique opportunity to study genetic variation across a diverse and well-characterised population.
The results show that around 2 per cent of sperm from men in their early 30s carried disease-causing mutations, but this rises to 3–5 per cent of sperm from middle-aged (43 to 58 years) and older men (59 to 74 years). Whilst men may be more likely to father children at a younger age, the researchers found that in those aged 70, 4.5 per cent of sperm carry disease-causing mutations. This clear age-related rise highlights how genetic risks for offspring increase as fathers get older.
This risk is driven not just by the steady build-up of random changes in DNA, but by a subtle form of natural selection acting on the sperm-producing cells in the testes, giving some mutations a competitive edge during sperm production.
The researchers identified 40 genes where certain changes in DNA are favoured during sperm production, including many linked to childhood diseases, severe neurodevelopmental disorders and inherited cancer risk. While 13 genes have already been associated with this process, the new findings show it is far more widespread than previously understood, affecting a broad range of genes important for cell growth and development.
Although the proportion of sperm carrying harmful mutations increases with age, not all of these changes lead to successful fertilisation or live births. Some may impair fertilisation, embryo development, or result in pregnancy loss. Further research is needed to understand exactly how the growing burden of sperm mutations translates into health outcomes for children.
The researchers hope that uncovering how variations in DNA arise and are shaped by selection in sperm will help improve reproductive risk assessment and open new opportunities to study how environmental and lifestyle factors impact genetic risks in future generations.
In a complementary study, also published in Nature today, 4 scientists from Harvard Medical School and the Sanger Institute investigated the same phenomenon from a different angle by looking at mutations already passed on to children, rather than those measured directly in sperm. By analysing DNA from over 54,000 parent–child trios and 800,000 healthy individuals, the team identified more than 30 genes where mutations give sperm cells a competitive edge, again including many linked to rare developmental disorders and cancer, and many overlapping the set of genes observed directly in sperm. The study found that these mutations can increase sperm mutation rates roughly 500-fold which helps explain why some rare genetic disorders appear when parents do not carry the mutations in their own DNA. Interestingly, the study notes that as these mutations are common in the sperm, it may look like some genes cause false-positive disease association due to the elevated mutation rate rather than a true disease link. The work highlights how natural selection within sperm can be directly observed in the DNA of children, influencing their chances of inheriting certain genetic disorders.
“We expected to find some evidence of selection shaping mutations in sperm. What surprised us was just how much it drives up the number of sperm carrying mutations linked to serious diseases.”
Dr Matthew Neville, first author at the Wellcome Sanger Institute
“Our findings reveal a hidden genetic risk that increases with paternal age. Some changes in DNA not only survive but thrive within the testes, meaning that fathers who conceive later in life may unknowingly have a higher risk of passing on a harmful mutation to their children.”
Professor Matt Hurles, Director of the Wellcome Sanger Institute and co-author
“We are incredibly grateful to the twins who took part in this study. By working with the TwinsUK cohort, we could include valuable longitudinal samples linked to rich health and genetic information, allowing us to explore how mutations accumulate and evolve with age in healthy individuals. This collaboration highlights the power of large, population-based cohorts for advancing our understanding of human development and inheritance.”
Professor Kerrin Small, co-author and Scientific Director of the TwinsUK study at King’s College London
“There’s a common assumption that because the germline has a low mutation rate, it is well protected. But in reality, the male germline is a dynamic environment where natural selection can favour harmful mutations, sometimes with consequences for the next generation.”
Dr Raheleh Rahbari, senior author and Group Leader at the Wellcome Sanger Institute
More information
Notes to Editors
- Launched in 2021 by the Wellcome Sanger Institute, nanorate sequencing (NanoSeq), is a method that makes it possible to study how genetic changes occur in human tissue whilst maintaining high accuracy. The method reduces error rates to less than five errors per billion calls which is much lower than typical somatic mutation rates.
- Blood samples were taken to ensure that mutations studied in sperm were only in sperm cells.
- The researchers split the data into age groups: 26–42 years (younger men), 43–58 years (middle-aged), and 59–74 years (older men).
- Seplyarskiy, V. et al. (2025) ‘Hotspots of human mutation point to clonal expansions in spermatogonia’. Nature. DOI: 10.1038/s41586-025-09579-7
- In a complementary study (Lawson, A. et al) researchers at the Sanger Institute have reported using targeted NanoSeq to uncover hidden mutations that occur naturally in bodies, providing insight into the earliest steps of cancer development and the role of mutations in different diseases. This team also collaborated with the TwinsUK study at King’s College London. They applied targeted NanoSeq to cheek and blood samples from more than 1,000 volunteers to uncover a rich landscape of mutations in healthy tissues, which can be applied to future research into ageing and diseases. Targeted NanoSeq is the same tool used in the above study. DOI: 10.1038/s41586-025-09584-w
Publication
Neville, M. et al. (2025) ‘Sperm sequencing reveals extensive positive selection in the male germline.’ Nature. DOI: 10.1038/s41586-025-09448-3
Funding
This research is part-funded by Wellcome. A full list of funders can be found in the acknowledgements in the publication.