IBS biomarker identified that could help personalise diet and treatment
Specific gut bacteria could be used as biomarkers to identify people with Irritable Bowel Syndrome (IBS) − a poorly understood, common, and often debilitating condition − who will benefit from a low FODMAP diet, new research has found. These findings are helping to shed light on the mechanisms behind IBS and potentially provide new treatment options for those affected.
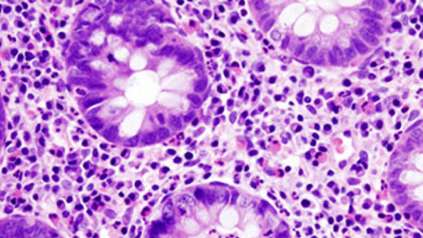
The new study, from the Wellcome Sanger Institute, the University of Cambridge, and Addenbrooke’s Hospital, used in-depth microbiome analysis to gain insight into this condition and found that people with IBS can be divided into two groups with different make ups of gut bacteria.
The research, published today (22 November 2021) in Gut, describes one group, making up approximately half of all patients, that had a distinctive and abnormal profile to their gut bacteria. This group benefitted greatly from a low FODMAP diet, which avoids certain foods including some fruits and vegetables, milk, and wheat.
Interestingly this improvement correlated with a shift in the gut bacteria towards a much more normal, ‘healthy’ profile. The researchers suggest that in the future these bacteria could be used as a biomarker to identify who will be more likely to benefit from this diet.
Having a more in-depth understanding of the link between these IBS-causing bacteria and the foods that trigger symptoms could allow people to have tailored treatment plans. In addition to this, understanding more about the bacteria that cause issues in some people could provide a new target for IBS therapies.
“IBS affects roughly 1 in 10 people globally, with limited effective therapies. The condition often has a huge impact on quality of life and it’s only been over the last decade or so, that research has started to investigate the potential mechanisms that are involved.”
Dr Stephen Moss, joint first author and Consultant Gastroenterologist at Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Trust
The low FODMAP diet has been shown to improve IBS in many cases1. However, this diet is challenging to follow as it avoids certain fruits, vegetables, milk, and wheat products and often requires individuals to spend more time planning and preparing their food, along with having fewer options for convenience food.
Due to these challenges, there is a need to better understand how these diets work and who is more likely to benefit, to ensure that those following or considering this are making an informed decision.
Through a unique study design, where patients and those who lived with them were investigated, and in-depth genomic and functional analysis that was made possible by technology at the Wellcome Sanger Institute, researchers were able to investigate the bacteria in 112 participants’ microbiomes in unmatched precision.
This novel research identified two distinct microbiome profiles in people with IBS. In one group, the bacterial makeup of the gut was similar to healthy individuals while the second group, known as IBSP, was different.
Both groups and anyone they lived with committed to a low FODMAP diet for four weeks, and while 75 per cent of overall cases in this study improved with the diet, those with an IBSP microbial profile had a dramatic change in their gut bacteria. After the four weeks, those with IBSP had a microbiome that resembled a healthy individual, and these individuals reported a higher degree of symptom improvement.
“Functional, genomic and mechanistic analyses have allowed us to uncover more about which bacteria are potentially contributing to IBS and also which metabolites are involved. We are hopeful that this research could lead to a personalised approach to IBS, which is supported by genomic research. We would like to thank the participants in this study for taking part, as our research would not have been possible without them.”
Dr Kevin Vervier, joint first author and Senior Staff Scientist at the Wellcome Sanger Institute
While it is possible to use the IBSP microbiome profile to identify those who would likely benefit from the low FODMAP diet, further research is required to understand more about the link between the bacteria found in those with IBSP and IBS symptoms to see if these bacteria could be a new target for IBS therapies. Closer study of the implicated bacteria may give the opportunity to better understand the interaction between diet, microbiota, metabolites and the human gut-brain axis that leads to the development of IBS symptoms in more than 10 per cent of the world’s population.
“The low FODMAP diet has previously shown to improve many of the symptoms of IBS, but very little is known about why this happens, or why some people respond better to it than others. Through our research, we were able to identify a biomarker that makes it possible to stratify different types of IBS and then identify who would benefit most from this diet. This is potentially very useful in ensuring that patients don’t undergo this restrictive and challenging diet without benefits.”
Professor Miles Parkes, joint senior author and Consultant Gastroenterologist at Addenbrooke’s Hospital, part of Cambridge University Hospitals NHS Trust
“IBS is a condition that affects thousands of people every day, yet the way that the gut microbiome and IBS symptoms are linked is still poorly understood. Our research dives deeper into the role of certain gut bacteria in possible IBS symptoms and gives a more precise view of what is going on. By understanding the role of these bacteria it could lead to new targeted therapies for those living with IBS.”
Dr Trevor Lawley, joint senior author and Group Leader at the Wellcome Sanger Institute
More information
- Whelan K, Martin LD, Staudacher HM, Lomer MCE. The low FODMAP diet in the management of irritable bowel syndrome: an evidence-based review of FODMAP restriction, reintroduction and personalisation in clinical practice. (2018). J Hum Nutr Diet. DOI: 10.1111/jhn.12530.
Publication:
K. Vervier, S. Moss, N. Kumar, et al. Two microbiota subtypes identified in irritable bowel syndrome with distinct responses to the low FODMAP diet. (2021). Gut. DOI: 10.1136/gutjnl-2021-325177
Funding:
This research was co-funded by Addenbrooke’s Charitable Trust (ACT), Cambridge and the Wellcome Sanger Institute and supported by the NIHR Cambridge Biomedical Research Centre.