Genetic mutations warn of skin cancer risk
Every year in the UK, almost 12,000 people are diagnosed with melanoma, a form of skin cancer. About 1 in 20 people with melanoma have a strong family history of the disease. In these patients, pinpointing the genetic mutations that drive disease development allows dermatologists to identify people who should be part of melanoma surveillance programmes.
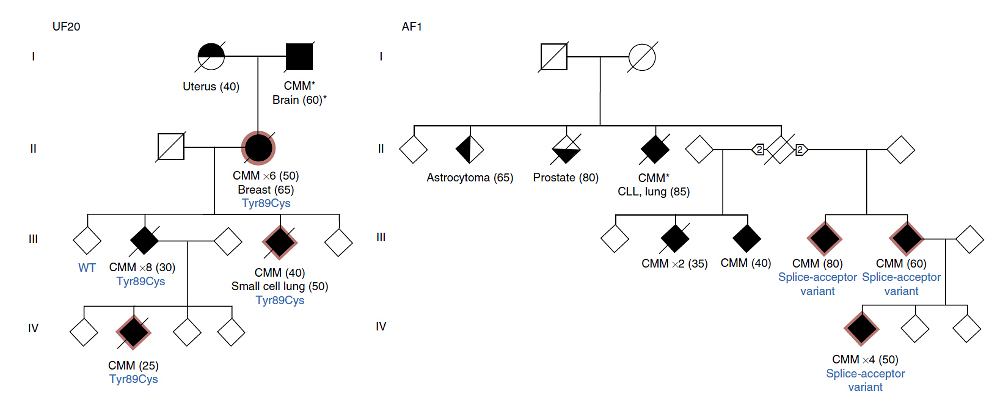
The team found that people with specific mutations in the POT1 gene were extremely likely to develop melanoma. These mutations deactivate the POT1 gene that protects the ends of our chromosomes from damage.
“Genomics is on the verge of transforming the healthcare system – this study highlights the potential clinical benefits that can be gained through genomic studies and offers potential strategies to improve patient care and disease management. With this discovery we should be able to determine who in a family is at risk, and in turn, who should be regularly screened for early detection.”
Dr David Adams Co-senior author from the Wellcome Trust Sanger Institute
Known genetic mutations account for approximately 40 per cent of all occurrences of inherited forms of melanoma. The team set out to identify the hereditary mutations that account for the other ~60 per cent by sequencing part of the genome of 184 patients with hereditary melanoma caused by unknown mutations.
They found that the inactivation of POT1 caused by these mutations leads to longer and potentially unprotected telomeres, regions at the end of our chromosomes that protect chromosomes from damage.
“This finding significantly increases our understanding of why some families have a high incidence of melanoma. Since this gene has previously been identified as a target for the development of new drugs, in the future, it may be possible that early detection will facilitate better management of this disease.”
Professor Tim Bishop Director of the Leeds Institute of Cancer and Pathology
The team also found that there were also cases of other cancer types in families with these hereditary mutations such as leukaemias and brain tumours. It seems that mutations that deactivate the POT1 gene may underlie other cancers, not just melanoma.
“Our research is making a real difference to understanding what causes melanoma and ultimately therefore how to prevent and treat melanoma and is a prime example of how genomics can transform public health. This study would not have been possible without the help and patience from the families that suffer from these devastating, inherited forms of melanoma.”
Professor Julia Newton Bishop Co-senior author from the University of Leeds
The team are currently working on developing cells and mice with an inactive POT1 gene. These will be used to test potential drug therapies that alter telomere metabolism.
“This is a step forward for people with a strong family history of melanoma, the most dangerous form of skin cancer. But it’s important to remember that, for most of us, avoiding sunburn and sunbeds is the best way to reduce the risk of this disease.”
Dr Safia Danovi Cancer Research UK’s senior science communications officer
More information
Funding
A full list of funding can be found in the paper.
Participating Centres
- Experimental Cancer Genetics, Wellcome Trust Sanger Institute, Hinxton, UK.
- Section of Epidemiology and Biostatistics, Leeds Institute of Cancer and Pathology, University of Leeds, Leeds, UK.
- Departamento de Bioquímica y Biología Molecular, Instituto Universitario de Oncología del Principado de Asturias (IUOPA), Universidad de Oviedo, Oviedo, Spain.
- Oncogenomics Laboratory, QIMR Berghofer Medical Research Institute, Herston, Brisbane, Queensland, Australia.
- Centre for Cancer Genetic Epidemiology, Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK.
- Molecular Epidemiology Laboratory, QIMR Berghofer Medical Research Institute, Herston, Brisbane, Queensland, Australia.
- Genetic Epidemiology Laboratory, QIMR Berghofer Medical Research Institute, Herston, Brisbane, Queensland, Australia.
- Statistical Genetics, Wellcome Trust Sanger Institute, Hinxton, UK.
- Laboratory of Translational Genomics, National Cancer Institute, Bethesda, Maryland, USA.
- Centre for Cancer Genetic Epidemiology, Department of Oncology, University of Cambridge, Cambridge, UK.
- Department of Dermatology, Leiden University Medical Centre, Leiden, The Netherlands.
Publications:
Selected websites
University of Leeds
The University of Leeds is one of the largest higher education institutions in the UK and a leading research powerhouse. It is a member of the Russell Group of research-intensive universities.
Cancer Research UK
- Cancer Research UK is the world’s leading cancer charity dedicated to saving lives through research.
- Cancer Research UK’s pioneering work into the prevention, diagnosis and treatment of cancer has helped save millions of lives.
- Cancer Research UK receives no government funding for its life-saving research. Every step it makes towards beating cancer relies on every pound donated.
- Cancer Research UK has been at the heart of the progress that has already seen survival rates in the UK double in the last forty years.
- Cancer Research UK supports research into all aspects of cancer through the work of over 4,000 scientists, doctors and nurses.
- Together with its partners and supporters, Cancer Research UK’s vision is to bring forward the day when all cancers are cured.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


