Final chapter to 60 year old blood group mystery
Researchers have uncovered the gene at the root of a human blood group that has remained a mystery for the past 60 years. They showed that a genetic deletion on this gene is responsible for the lack of this blood group in some people.
With the discovery of the gene behind the Vel blood group, medical scientists can now develop a more reliable DNA test to identify people who lack this group. This will reduce the risk of severe, and sometimes life threatening, destruction of the Vel-positive donor red blood cells in patients with antibodies against Vel.
The genetic basis of nearly all 34 blood group systems has been resolved over the past century, but identification of the underlying gene of the Vel blood group has withstood persistent attempts since it was first identified 60 years ago. It is estimated that one in 5000 people are Vel-negative, and routine blood transfusions for patients with antibodies against Vel can lead to kidney failure and even death.
“This is really exciting as it shows how the power of modern genomics technologies can directly benefit patient care. This is also a milestone in blood group genetics and the end of long and astounding journey of discoveries in blood group genetics which started with Landsteiner from Austria and Fisher, Coombs and Morgan from England.”
Professor Willem Ouwehand who heads one of the NHS Blood and Transplant research teams at both the University of Cambridge and the Wellcome Trust Sanger Institute
The discovery by the team would not have been possible without the colleagues from the blood transfusion services of Denmark, England and the Netherlands who undertook the Herculean effort of identifying the 65 individuals that lacked the Vel blood group by testing the red blood cells from nearly 350,000 donors with antibodies against Vel.
They then sequenced the coding fraction of the genomes of five donors who lack the Vel group to identify the underlying gene.
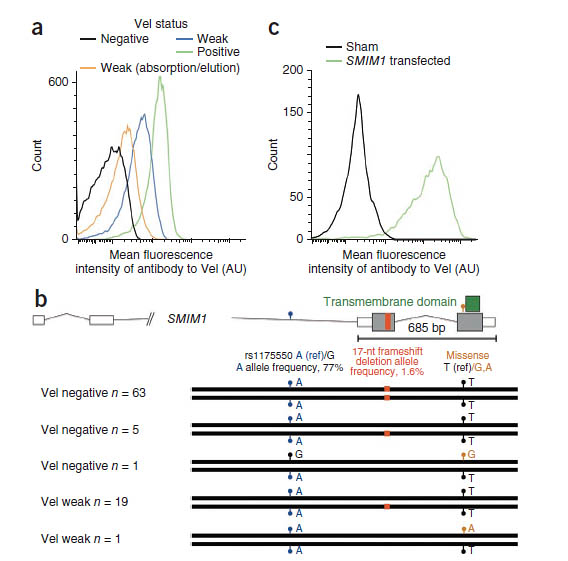
The team showed that the gene SMIM1 malfunctions in Vel-negative people. SMIM1 is found on chromosome 1 and specifies a small protein, five times smaller than the average human protein. This provides a direct explanation why a discovery by other routes has proven so challenging.
“It has been a remarkable feat to go from gene discovery to function in less than two months.”
Professor Ouwehand
Current testing for Vel-negative people can be inaccurate but identifying this new role for the gene will make it easier to identify people who lack Vel. The Sanquin Blood Supply research laboratories in Amsterdam and the NHS Blood and Transplant Centre in Cambridge are currently working together to develop a new and affordable DNA test to efficiently identify people who lack the Vel group.
“We already knew of 75 genomic regions that are associated with the haemoglobin levels and other red blood cell traits But we quickly realised that the SMIM1 gene identified in our study is the same as one of these associated regions. We had already assumed that a gene in this region of chromosome 1 played a role in the life of red blood cells, but we now have conclusive evidence that it is SMIM1.
“We have shown that this gene controls a protein in the membrane of red blood cells. Switching off the SMIM1 gene in zebrafish showed a remarkable reduction in the number of red cells formed and caused anaemia in the fish.”
Dr Pim van der Harst from Groningen University in the Netherlands who led the GWAS analysis for red cell traits in nearly 100,000 individuals
The team observed that the common variant identified by the red blood cell study has a strong effect on how well the SMIM1 gene functions. This not only explains why the level of the Vel blood group varies so extensively in the population, but is also makes it extremely plausible that the Smim1 protein influences haemoglobin levels of red blood cells.
A low haemoglobin level confers a risk of anaemia, which is one of the most frequent reasons for an individual to visit their doctor. The team are pursuing further research to deduce how Smim1 protein regulates red blood cell formation.
“As the molecular machinery underlying red blood cell formation has been researched for decades in fish, mice and man, our discovery that a gene which was considered hypothetical until recently actually controls a red blood cell membrane protein with an important role in the regulation of haemoglobin levels is astonishing. A better understanding of how the SMIM1 gene is regulated is important and this effort will greatly benefit from the Blueprint project which will be releasing its results on the biology of blood cells and their precursors this year.”
Professor Ellen van der Schoot from the Sanquin research laboratories in Amsterdam
“We have worked for nearly a decade to identify the donors across England that lack the Vel blood group so that we can provide matched and safe blood to patients with antibodies against Vel. The discovery of the SMIM1 gene was achieved so quickly and it is truly amazing to see how medical genomics is changing the care landscape for NHS patients.”
Mr Malcolm Needs from NHS Blood and Transplant in Tooting London
More information
Funding
This study was supported by the British Heart Foundation, European Commission, Medical Research Council, National Institute for Health Research, NHS Blood and Transplant and the Wellcome Trust.
Participating Centres
- Department of Haematology, University of Cambridge, Cambridge, UK.
- Wellcome Trust Sanger Institute, Wellcome Trust Genome Campus, Hinxton, Cambridge, UK.
- Department of Experimental Immunohaematology, Sanquin Research, Amsterdam, The Netherlands.
- Landsteiner Laboratory, Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands.
- National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre, Cambridge, UK.
- National Health Service (NHS) Blood and Transplant, Cambridge, UK.
- European Molecular Biology Laboratory (EMBL)–European Bioinformatics Institute, Wellcome Trust Genome Campus, Hinxton, Cambridge, UK.
- Department of Hematopoiesis, Sanquin Research, Amsterdam, The Netherlands.
- Department of Genetics, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands.
- NHS Blood and Transplant, Tooting, London, UK.
- Department of Cardiology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands.
- Houghton St, Somerville, Massachusetts, USA.
- Department of Molecular Biology, Faculty of Science, Nijmegen Centre for Molecular Life Sciences, Radboud University, Nijmegen, The Netherlands.
- International Blood Group Reference Laboratory, NHS Blood and Transplant, North Bristol Park, Northway, Filton, Bristol, UK.
- Medical Research Council (MRC) Biostatistics Unit, Institute of Public Health, Cambridge, UK. 16Department of Clinical Immunology, Rigshospitalet, Copenhagen University Hospital, Copenhagen, Denmark.
- Department of Experimental Hematology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands.
- Department of Stem Cell Biology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands.
- Laboratory of Genetic, Endocrine and Metabolic Diseases, Department of Laboratory Medicine, Radboud University Medical Centre, Nijmegen, The Netherlands.
- Department of Human Genetics, Radboud University Medical Centre, Nijmegen, The Netherlands.
Publications:
Selected websites
NHS Blood and Transplant
NHS Blood and Transplant (NHSBT) is a joint England and Wales Special Health Authority. Its remit includes the provision of a reliable, efficient supply of blood and associated services to the NHS in England and North Wales. It is also the organ donor organisation for the UK and is responsible for matching and allocating donated organs. Eight research themes make up NHSBT’s planned Research & Development Strategy. The main research sites, in collaboration with University partners, are Cambridge, Oxford, London and Bristol, with specialist activity in Birmingham and Liverpool.
University of Cambridge
The mission of the University of Cambridge is to contribute to society through the pursuit of education, learning and research at the highest international levels of excellence. It admits the very best and brightest students, regardless of background, and offers one of the UK’s most generous bursary schemes. The University of Cambridge’s reputation for excellence is known internationally and reflects the scholastic achievements of its academics and students, as well as the world-class original research carried out by its staff. Some of the most significant scientific breakthroughs occurred at the University, including the splitting of the atom, invention of the jet engine and the discoveries of stem cells, plate tectonics, pulsars and the structure of DNA. From Isaac Newton to Stephen Hawking, the University has nurtured some of history’s greatest minds and has produced more Nobel Prize winners than any other UK institution with over 80 laureates.
Sanquin Blood Supply Foundation
The Sanquin Blood Supply Foundation in the Netherlands ensures the safe and efficient blood and platelet supply for the Dutch Healthcare system. Sanquin also develops and produces pharmaceutical products, conducts high-quality scientific research, and develops and performs a multitude of diagnostic services.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


