Elusive platelet count and limb development gene discovered
Researchers have identified an elusive gene responsible for Thrombocytopenia with Absent Radii (TAR), a rare inherited blood and skeletal disorder. As a result, this research is now being transformed into a medical test that allows prenatal diagnosis and genetic counselling in affected families.
The team used genetic sequencing to discover that TAR results from low levels of the protein called Y14. They found that the syndrome occurs by an unique inherited mechanism.
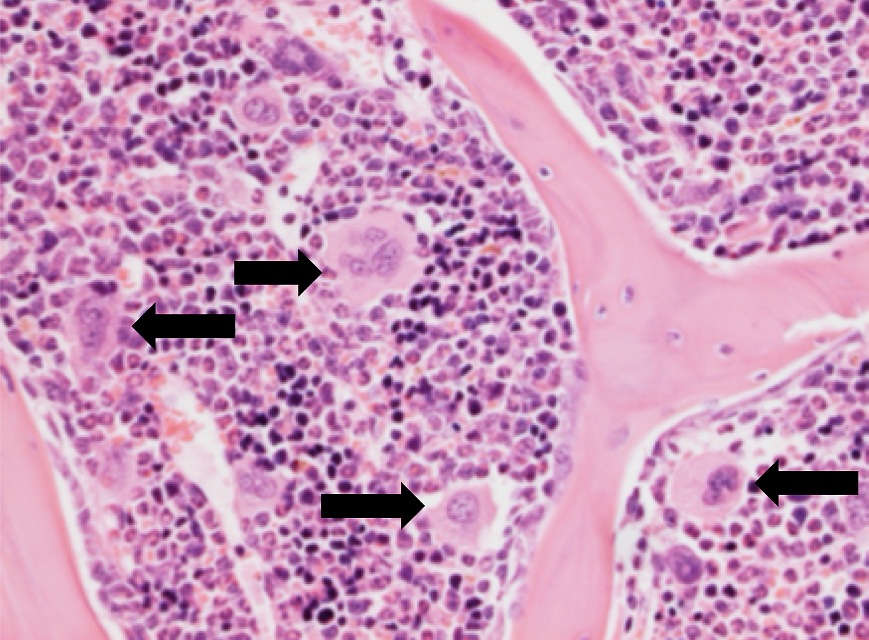
Platelets are the second most abundant cell in the blood. Their main task is to survey the blood vessel wall for damage and to plug and repair it where required. Some people are born with low numbers of platelets and these rare conditions are thought to be inherited. TAR syndrome combines the unique features of low platelet count and prominent bleeding, especially in infancy, and skeletal abnormalities affecting the upper limb ranging from absence of the radial bone in the forearm to virtually total absence of upper limb. The genetic basis of TAR syndrome has eluded researchers for 50 years.
“Without the use of modern genomics technologies, the discovery of this unexpected mechanism of disease inheritance would have been much more difficult. To achieve our latest findings, we deciphered about 40 million letters of genetic code in five patients.”
Dr Cornelis Albers from the Sanger Institute and the University of Cambridge
Many people with TAR were known to have a deletion in one copy of chromosome 1, but this was thought not to be the whole story because parents who carry the same deletion are not suffering from TAR: other variants had to be involved. The team sequenced the genomes of people affected by the disorder who also carried the deletion and discovered that the vast majority of them had one of two variants of a gene called RBM8A. They found that when the genetic deletion and one of the variants are co-inherited by a child, TAR results.
RBM8A controls the production of the protein Y14. They found that the combination of the genetic deletion of one copy of the RBM8A gene and the variants on the other copy greatly reduces the level of Y14. The team concluded that it is low levels of Y14 that affect platelet formation and cause TAR disorder.
“The lack of production of adequate amounts of the protein Y14 in TAR patients only seems to effect the formation of platelets but not of other blood cells. We have shed some light on how some inherited disorders can present with such striking features associating seemingly unconnected characteristics such as skeletal and blood defects.”
Dr Cedric Ghevaert from the University of Cambridge
This is the first human disorder identified to be caused by a presumed defect of the Exon Junction Complex Part of the cellular machinery that contributes to producing messages that direct protein production. This study opens the path that could lead to the identification of the genetic basis of other similar inherited syndromes, which will help improvements in diagnosis, genetic counselling and patient care in the NHS and beyond.
“The discovery of the gene for TAR will make it simpler to diagnose more accurately future cases with a simple DNA test. This new test is currently being developed for the NHS as part of the international ThromboGenomics initiative led by Professor Ouwehand.”
Dr Ruth Newbury-Ecob, Honorary Reader in Medical Genetics and Consultant in Clinical Genetics at the University of Bristol Hospitals
More information
The findings were made following a collaborative study by the NHS Blood and Transplant platelet research team at the University of Cambridge and the Wellcome Trust Sanger Institute, which is led by Dr Cedric Ghevaert and Professor Willem Ouwehand. The Cambridge researchers joined forces with Dr Ruth Newbury-Ecob from the University of Bristol and worked together with various other European research partners from Belgium, France, Germany and the Netherlands.
Funding
The platelet research team in Cambridge is supported by the British Heart Foundation, the European Commission, the National Institute for Health Research for England (NIHR), NHS Blood and Transplant and the Wellcome Trust.
Publications:
Selected websites
NHS Blood and Transplant
Dr Cedric Ghevaert and Prof Willem Ouwehand are also consultant Haematologists for NHS Blood and Transplant (NHSBT). NHSBT collects blood and platelets from non-remunerated volunteer donors. Every day about 8,000 units of blood are needed by the NHS and 1100 platelet concentrates. For the latter about 600 donors attend a special clinic at which platelets are harvested from the blood of the donor by a process called apheresis.
The National Institute for Health Research
The National Institute for Health Research (NIHR) provides the framework through which the research staff and research infrastructure of the NHS in England is positioned, maintained and managed as a national research facility. The NIHR provides the NHS with the support and infrastructure it needs to conduct first-class research funded by the Government and its partners alongside high-quality patient care, education and training. Its aim is to support outstanding individuals (both leaders and collaborators), working in world-class facilities (both NHS and university), conducting leading-edge research focused on the needs of patients.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


