Genome of emerging antibiotic resistant bacteria decoded
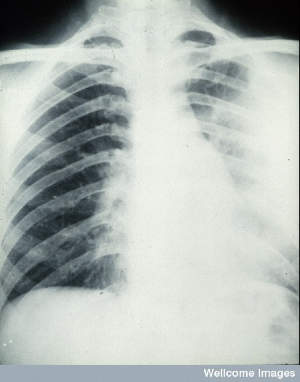
While not well known to the public, Klebsiella pneumoniae has recently been highlighted by the UK Chief Medical Officer, the European Centre for Disease Prevention and Control and the World Health Organization as an urgent and immediate threat to health. K. pneumoniae can cause a wide range of acute infections such as meningitis and pneumonia. In lower-income countries, the bacteria are one of the most common causes of bloodstream infections in infants and a leading cause of premature deaths. It is hoped that this data set, comprised of whole genome sequences of nearly 300 plant, bovine and human samples from around the world, will increase understanding of the bacterium and help scientists to track rapidly evolving antibiotic resistance across different species and lineages.
“For too long with Klebsiella, we have focussed on single lineages. We will now be able to recognise emerging lineages from a huge cloud of Klebsiella diversity, helping us to follow and tackle drug resistance in this increasingly dangerous pathogen.”
Professor Nick Thomson Corresponding author from the Wellcome Trust Sanger Institute
Researchers found that the distribution of genes responsible for conferring drug resistance varied according to the geographical origin of the sample, not according to the specific strain of K. pneumoniae. This shows that evolution of the pathogen is directly linked to local antibiotic use and that these resistance elements regularly transfer between different strains.
Most drug resistance genes were discovered in samples from patients with infections they acquired while receiving treatment for another illness in hospital, or from people who carried the bacteria without showing any symptoms of infection. These strains are generally less infectious and unlikely to affect a healthy individual. However, researchers are concerned, given the ease with which different strains of the bacteria can share genetic information, that antibiotic resistance genes may soon appear in more virulent Klebsiella strains, creating an untreatable and highly infectious bacterial population.
“Almost any Klebsiella pneumoniae can cause an infection in someone who is already ill in hospital, but very few strains are virulent enough to affect a healthy person. So far we have been extremely lucky in that most of the antibiotic-resistant strains are not highly virulent to humans. Unfortunately, Klebsiella strains are very good at swapping around genes that encode antibiotic resistance, so it’s probably just a matter of time before we see strains that have the dreaded combination of virulence and antibiotic resistance.”
Dr Kathryn Holt First author from The University of Melbourne
Currently, antibiotic resistance genes are monitored in hospital laboratories; this research demonstrates the importance of also tracking the genes that determine how virulent a strain is. In this study, researchers found that many of the most strains of K. pneumoniae that were virulent enough to cause serious infections in people who weren’t already ill in hospital, contain genes that help them to steal iron away from human cells. Iron is essential for bacteria to replicate, so these organisms are better able to compete for iron and replicate more easily during a human infection, where iron is scarce. This feature makes them more able to infect healthy hosts and, when tested for, could help researchers to identify and track hypervirulent strains.
The study also provides a foundation for further studies into how these bacteria adapt to new niches and how they become more diverse. Active surveillance for virulence genes and antibiotic resistance will also be crucial as the prevalence of this pathogen continues to rise.
“In Asia, K. pneumoniae infections are becoming increasingly common and increasingly associated with mortality. If the trends we are seeing here in Vietnam and across Asia continue, drug-resistant Klebsiella will become an even more predominant and an exceptionally dangerous pathogen.”
Professor Stephen Baker An author from the Oxford University Clinical Research Unit in Vietnam
More information
Funding
This work was funded by: the NHMRC of Australia, fellowship #628930 and #1061409, program grant #606788; the Wellcome Trust, grant #098051 to Wellcome Trust Sanger Institute, grant #089275/H/09/Z for the Oxford-Mahosot Hospital-Wellcome Trust Research Unit, Sir Henry Dale Fellowship (co-funded by the Royal Society); the Victorian Life Science Computation Initiative grant #VR0082.
Participating Centres
A full list of participating centres can be found on the paper.
Publications:
Selected websites
University of Melbourne
Established in 1853, the University of Melbourne is a public-spirited institute that makes distinctive contributions to society in research, learning and teaching and engagement. It’s consistently ranked among the leading universities in the world, with international rankings of world universities placing it as number 1 in Australia and number 33 in the world (Times Higher Education World University Rankings 2014-2015).
Oxford University Clinical Research Unit
Oxford University Clinical Research Unit in Viet Nam (OUCRU) was established in 1991 and is one of the Wellcome Trust Major Overseas Programmes. It is based within the Ho Chi Minh City (HCMC) Hospital for Tropical Diseases (HTD), at tertiary referral hospital for infectious diseases for southern Viet Nam, under the direction of the Health Service of Ho Chi Minh City and the Ministry of Health. OUCRU also has a base in the capital Hanoi at the National Institute of Infectious & Tropical Diseases (NHTD) and has satellite research units in Kathmandu (Nepal) and Jakarta (Indonesia). OUCRU has a large clinical and scientific research programme which focuses on the most significant infectious diseases in Viet Nam. Many of these are also among the greatest threats to global health in the 21st century. The work covers clinical research and aspects of immunology, host and pathogen genetics, molecular biology, virology, mathematical modelling, bioinformatics, biostatistics and epidemiology. The research is supported by its extensive Clinical Trials Unit and Data Management Centre.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


