Biology behind blood trait signals
Researchers at the Wellcome Trust Sanger Institute and University of Cambridge have unpicked genetic variants that affect the formation of blood cells. They found that around a third of the variants play a role in gene regulation, and that the action of these variants is specific to individual cell types. The discovery is an important step towards unravelling the biological mechanisms behind variants identified in genome-wide scans of blood traits.
Nearly three-quarters of the variants associated with red blood cell and platelet formation lie in non-protein coding regions of the genome. The team believed that many of these variants are likely to be involved in gene regulation. In cells, DNA is tightly wrapped around proteins to form a structure called chromatin. Regions that regulate genes – so called ‘regulatory elements’ – are often located in regions of ‘open chromatin’, where they are accessible for protein binding.
To study this in more detail, the team investigated genetic variants from genome-wide scans involving more than 100,000 individuals. These studies looked at several blood cell traits, including the size of red blood cells and the volume of platelets. These traits are commonly used in the clinic as indicators of health and disease.
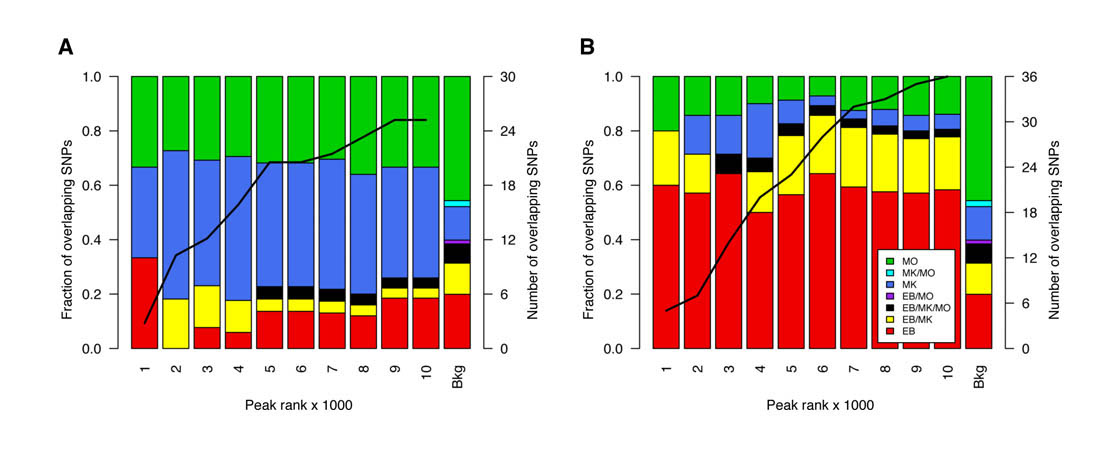
The researchers mapped regions of open chromatin in several human blood cell types, to determine whether the variants associated with blood cell traits fell into these regulatory regions.
“We wanted to investigate whether we could use this approach to better understand genetic signals associated with the formation of blood cells. We looked at over 140 variants associated with different blood cell traits and found that these genetic signals were enriched in regulatory regions specific to each different blood cell type.”
Dr Dirk Paul First author from the Wellcome Trust Sanger Institute
The researchers then focused on 13 genetic variants associated with platelet formation, finding that 10 of the variants acted by either creating or disrupting sites of protein binding. The results suggest a common mechanism through which regulatory variants may act – by altering the binding of proteins important for transcription.
The team further extended the list of regulatory variants by studying the contribution of weaker association signals, those that did not reach the threshold of significance for genome-wide scans. The results suggest that even weaker association signals may be biologically relevant if located in open chromatin regions, and should be considered in later functional studies.
“Genome-wide association studies have been extremely successful in allowing us to identify regions of the genome that are linked to a specific trait. We can now go one step further with this approach, and start assigning functional information to these genetic signals.”
Professor Panos Deloukas Joint senior author from the Wellcome Trust Sanger Institute
“This effort will further benefit from the BLUEPRINT project, which will be releasing similar data sets from many other different blood cells and their precursors later this year.
“We hope this will reveal exciting biological insights into blood cell formation that can be used to improve our understanding of diseases. The success of our strategy is also giving us the confidence to look beyond blood traits to a range of different cell types and diseases.”
Professor Willem Ouwehand Joint senior author from the University of Cambridge
More information
http://www.blueprint-epigenome.eu/
Funding
A full list of funding can be found on the paper.
Participating Centres
- Wellcome Trust Sanger Institute, Hinxton, Cambridge CB10 1SA, United Kingdom
- UCL Cancer Institute, University College London, London WC1E 6BT, United Kingdom
- Department of Haematology, University of Cambridge and National Health Service (NHS) Blood and Transplant, Cambridge CB2 0PT, United Kingdom
- Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
- MRC Biostatistics Unit, Institute of Public Health, Cambridge CB2 0SR, United Kingdom
- NIHR Biomedical Research Centre, Cambridge CB2 0PT, United Kingdom
- Department of Cardiology, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
- Department of Genetics, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
- Department of Epidemiology and Biostatistics, Imperial College London, London W2 1NY, United Kingdom
- Imperial College Healthcare NHS Trust, Hammersmith Hospital, London W12 0HS, United Kingdom
- Royal Brompton and Harefield Hospitals NHS Trust, London SW3 6NP, United Kingdom
- Ealing Hospital NHS Trust, Southall, Middlesex UB1 3HW, United Kingdom
Publications:
Selected websites
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


