Emerging superbug genome sequenced
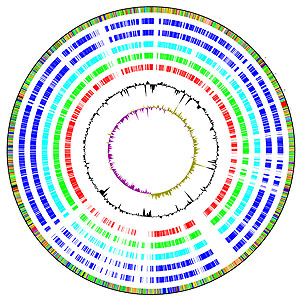
The genome of a newly-emerging superbug has just been sequenced – that of Stenotrophomonas maltophilia, commonly known as Steno. The results reveal an organism with a remarkable capacity for drug resistance. The research was carried out by scientists at the Wellcome Trust Sanger Institute near Cambridge and the University of Bristol.
Understanding the genome of Steno will enable researchers to discover how to deal with this particularly resistant organism. The paper will be published in Genome Biology.
“This is the latest in an ever-increasing list of antibiotic-resistant hospital superbugs. The degree of resistance it shows is very worrying. Strains are now emerging that are resistant to all available antibiotics, and no new drugs capable of combating these ‘pan-resistant’ strains are currently in development.”
Dr Matthew Avison from the University of Bristol and senior author on the paper
Pan-resistant Steno infections could even be as hard to treat as MRSA and C. difficile (known as Cdiff) infections. Although Steno is common in the environment, infections are rarer than those of MRSA and Cdiff and are exclusively hospital-acquired.
Steno flourishes in moist environments, such as around taps and shower heads, and so can be easily transferred to patients. A typical route of entry for this superbug is through catheters that are left in place for long periods of time. These long-dwelling catheters are used most often for seriously ill patients and some undergoing chemotherapy.
Steno can stick to the catheter and grow into a ‘biofilm’. When the catheter is next flushed, the Steno biofilm enters the patient’s bloodstream. If their immune system is impaired (which is often the case in the seriously ill and those undergoing chemotherapy) the organism can multiply and cause septicaemia. The gravity of this situation is highlighted by the results from the team since, as this new research shows, these septicaemic patients will often be treated with antibiotics to which Steno is largely resistant.
There are approximately 1000 reports of Steno being responsible for blood poisoning in the UK each year, with a mortality rate of about 30 per cent. The organism is also found in the lungs of many adults with cystic fibrosis, and causes ventilator-associated pneumonias, particularly in elderly intensive-care patients.
The key questions that need to be addressed are: How does Steno stick to surfaces like catheters and ventilator tubes? How does it form biofilms that make it resistant to our attempts to decontaminate and clean these devices? Why is it resistant to antibiotics?
“The genome sequence should help us to combat these properties. For example, if we know which proteins allow it to stick to surfaces, we could try to develop biochemical compounds that interfere with this interaction. If we understand its antibiotic resistance mechanisms, we might be able to design inhibitors that block them.”
Dr Lisa Crossman from the Sanger Institute and first author on the paper
While Fortunately, Steno infections are still relatively uncommon, they are on the increase. Furthermore, there are two other organisms that, like Steno, cause infections by colonising catheters and so on, but are more common.
“Genome sequences for these two also exist, and so now we can look at what they all have in common genetically that might explain why they all behave in a similar way in the hospital.”
Dr Matthew Avison from the University of Bristol
More information
Funding
This research was funded by the Wellcome Trust and the British Society for Antimicrobial Chemotherapy.
Publications:
Selected websites
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute, which receives the majority of its funding from the Wellcome Trust, was founded in 1992. The Institute is responsible for the completion of the sequence of approximately one-third of the human genome as well as genomes of model organisms and more than 90 pathogen genomes. In October 2006, new funding was awarded by the Wellcome Trust to exploit the wealth of genome data now available to answer important questions about health and disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


