Test run finds no cancer risk from stem cell therapy
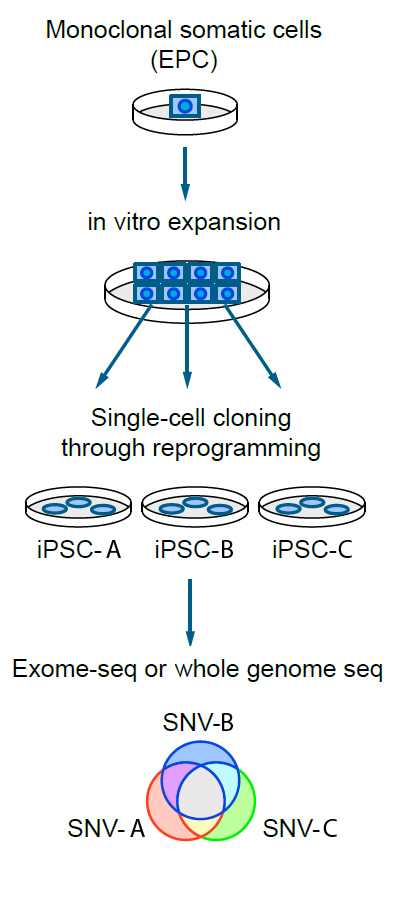
The iPSC cells are derived from the same original cell, so any mutations that they share (in the middle of the Venn diagram) are common to the original cells and so were acquired during the person’s life. Any mutations outside of the shared area of the Venn diagram were acquired only by that cell line during reprogramming and culturing.
It is the first time scientists have tracked the genetic mutations gathered by iPS cells as they are grown in the laboratory.
The idea behind the research was to follow the whole journey iPS cells will take when used in clinical therapy. The Sanger Institute team, led by Professor Allan Bradley and Dr Kosuke Yusa, started with blood cells donated by a 57-year-old man.
As a person grows from embryo, to child, to adult, and, as they age, the cells in their body generate a mosaic of tiny genetic changes. Most of these mutations have no effect but some can lead to cancer. The Sanger team traced the history of genetic changes in both the donated blood cell and the iPS cells created from it.
The results reveal mutations arise 10 times less often in iPS cells than they do in laboratory-grown blood cells and that none of the iPS cell mutations are in genes known to cause cancer.
“None of the mutations we found in induced pluripotent stem cells were cancer-driver mutations or mutations in cancer-causing genes. We didn’t find anything that would preclude the use of iPS cells in therapeutic medicine.”
Dr Foad Rouhani First author of the study, from the Wellcome Trust Sanger Institute
In addition, the team used the iPS cells, reprogrammed from the donated blood cell, to trace the history of every mutation that one cell had developed from the time it was a fertilised egg all the way up to the moment it was taken out of the body.
This is the first time that mutation rates of both types of cells, the donor cell and iPS cell, have been calculated and compared.
“Until now the question of whether generating iPS cells and growing them in cell culture creates mutations has not been addressed in detail. If human cells are really to be reprogrammed on a large scale for use in regenerative medicine then understanding the mutations the donor cells carry will be a crucial step. We now have the tools to do this.”
Professor Allan Bradley Co-senior author from the Sanger Institute
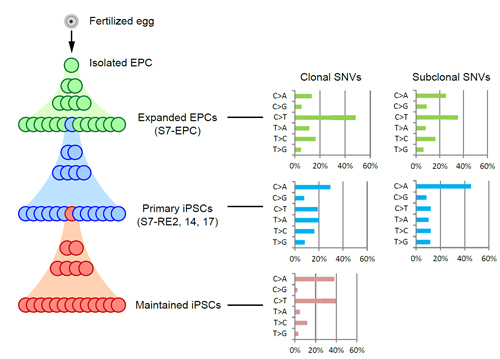
From living within the body, to being separated from the body and grown in the labotory, then being reprogrammed to an iPSC cell, and finally being maintained in laboratory-based culture.
To the right, the types DNA base pair changes that were found in the genomes of each type of cells when their genomes were sequenced.
“One of the exciting things is that we have found a way to use iPS cells as a tool to look at the genetic history of a single cell. It also underlines the fact that before you use these cells you really need to characterise them to a high degree to know where the mutations that have been introduced are.”
Dr Kosuke Yusa Co-senior author from the Sanger Institute
The team also found that the genetic changes that do take place in iPS cells in the lab might be caused by a mechanism known as oxidative stress. They hope this knowledge will help to find ways to improve the process of making iPS cells.
Researchers from the University of Cambridge and the European Bioinformatics Institute (EMBL-EBI) also contributed to the study.
More information
Publications:
Selected websites
About the University of Cambridge
The mission of the University of Cambridge is to contribute to society through the pursuit of education, learning and research at the highest international levels of excellence. To date, 90 affiliates of the University have won the Nobel Prize. Founded in 1209, the University comprises 31 autonomous Colleges, which admit undergraduates and provide small-group tuition, and 150 departments, faculties and institutions. Cambridge is a global university. Its 19,000 student body includes 3,700 international students from 120 countries. Cambridge researchers collaborate with colleagues worldwide, and the University has established larger-scale partnerships in Asia, Africa and America. The University sits at the heart of one of the world’s largest technology clusters. The ‘Cambridge Phenomenon’ has created 1,500 hi-tech companies, 14 of them valued at over US$1 billion and two at over US$10 billion. Cambridge promotes the interface between academia and business, and has a global reputation for innovation.
EMBL-EBI
The European Bioinformatics Institute is part of EMBL, and is a global leader in the storage, analysis and dissemination of large biological datasets. EMBL-EBI helps scientists realize the potential of ‘big data’ by enhancing their ability to exploit complex information to make discoveries that benefit mankind. It is a non-profit, intergovernmental organization funded by EMBL’s 21 member states and two associate member states. Its 570 staff hail from 57 countries, and work with a regular stream of visiting scientists throughout the year. EMBL-EBI is located on the Wellcome Genome Campus in Hinxton, Cambridge in the United Kingdom.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world’s leading genome centers. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programs and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Wellcome Trust
The Wellcome Trust is a global charitable foundation dedicated to achieving extraordinary improvements in human and animal health. We support the brightest minds in biomedical research and the medical humanities. Our breadth of support includes public engagement, education and the application of research to improve health. We are independent of both political and commercial interests.


