Artificial bile ducts successfully grown in lab and transplanted into mice could help treat liver disease in children
Cambridge scientists have developed a new method for growing and transplanting artificial bile ducts that could in future be used to help treat liver disease in children, reducing the need for liver transplantation.
In research published in the journal Nature Medicine, the researchers grew 3D cellular structure which, once transplanted into mice, developed into normal, functioning bile ducts.
The study suggests that it will be feasible to generate and transplant artificial human bile ducts using a combination of cell transplantation and tissue engineering technology. This approach provides hope for the future treatment of diseases of the bile duct; at present, the only option is a liver transplant.
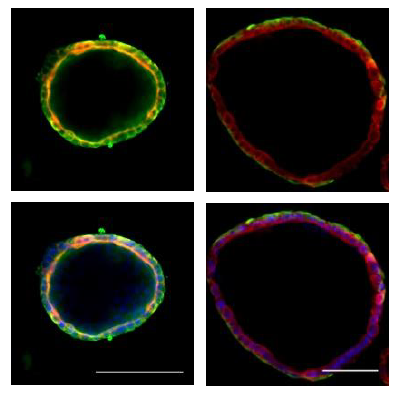
The University of Cambridge research team, led by Professor Ludovic Vallier and Dr Fotios Sampaziotis from the Wellcome – MRC Cambridge Stem Cell Institute and Dr Kourosh Saeb-Parsy from the Department of Surgery, extracted healthy cells (cholangiocytes) from bile ducts and grew these into functioning 3D duct structures known as biliary organoids. When transplanted into mice, the biliary organoids assembled into intricate tubular structures, resembling bile ducts.
The researchers, in collaboration with Mr Alex Justin and Dr Athina Markaki from the Department of Engineering, then investigated whether the biliary organoids could be grown on a “biodegradable collagen scaffold”, which could be shaped into a tube and used to repair damaged bile ducts in the body. After four weeks, the cells had fully covered the miniature scaffolding resulting in artificial tubes which exhibited key features of a normal, functioning bile duct. These artificial ducts were then used to replace damaged bile ducts in mice. The artificial duct transplants were successful, with the animals surviving without further complications.
“Our work has the potential to transform the treatment of bile duct disorders. At the moment, our only option is liver transplantation, so we are limited by the availability of healthy organs for transplantation. In future, we believe it will be possible to generate large quantities of bioengineered tissue that could replace diseased bile ducts and provide a powerful new therapeutic option without this reliance on organ transplants.”
Professor Ludovic Vallier Senior author of the paper from the Wellcome – MRC Cambridge Stem Cell Institute and a senior Group Leader at the Wellcome Trust Sanger Institute
“This demonstrates the power of tissue engineering and regenerative medicine. These artificial bile ducts will not only be useful for transplanting, but could also be used to model other diseases of the bile duct and potentially develop new drug treatments.”
Dr Fotios Sampaziotis First author on the paper, from the Wellcome – MRC Cambridge Stem Cell Institute
Professor Vallier is part of the Department of Surgery at the University of Cambridge and his team are jointly based at the Wellcome Trust – MRC Cambridge Stem Cell Institute and the Wellcome Trust Sanger Institute.
The support of the Medical Research Council, Sparks children’s medical research charity and the European Research Council has been invaluable in facilitating this research, and is gratefully acknowledged by Ludovic and the team.
More information
Funding:
This work was funded by the Medical Research Council, European Research Council and the Sparks children’s medical charity.
Publications:
Selected websites
Wellcome Trust - MRC Cambridge Stem Cell Institute
The Wellcome Trust – MRC Cambridge Stem Cell Institute is a world-leading centre for stem cell research with a mission to transform human health through a deep understanding of normal and pathological stem cell behaviour. Bringing together biological, clinical and physical scientists operating across a range of tissue types and at multiple scales, we explore the commonalities and differences in stem cell biology in a cohesive and inter-disciplinary manner. In 2018, we will relocate to a new purpose-built home on the Cambridge Biomedical Campus. Housing over 350 researchers, including a critical mass of clinician scientists, the Institute will integrate with neighbouring disease-focused research institutes and also act as a hub for the wider stem cell community in Cambridge.
The Wellcome Trust Sanger Institute
The Wellcome Trust Sanger Institute is one of the world's leading genome centres. Through its ability to conduct research at scale, it is able to engage in bold and long-term exploratory projects that are designed to influence and empower medical science globally. Institute research findings, generated through its own research programmes and through its leading role in international consortia, are being used to develop new diagnostics and treatments for human disease.
The Medical Research Council
The Medical Research Council has been at the forefront of scientific discovery to improve human health. Founded in 1913 to tackle tuberculosis, the MRC now invests taxpayers’ money in some of the best medical research in the world across every area of health. Twenty-nine MRC-funded researchers have won Nobel prizes in a wide range of disciplines, and MRC scientists have been behind such diverse discoveries as vitamins, the structure of DNA and the link between smoking and cancer, as well as achievements such as pioneering the use of randomised controlled trials, the invention of MRI scanning, and the development of a group of antibodies used in the making of some of the most successful drugs ever developed. Today, MRC-funded scientists tackle some of the greatest health problems facing humanity in the 21st century, from the rising tide of chronic diseases associated with ageing to the threats posed by rapidly mutating micro-organisms.
European Research Council (ERC)
The mission of the European Research Council (ERC) is to encourage the highest quality research in Europe through competitive funding and to support investigator-driven frontier research across all fields, on the basis of scientific excellence. The ERC complements other funding activities in Europe such as those of the national research funding agencies, and is a flagship component of Horizon 2020, the European Union's Research Framework Programme for 2014 to 2020.The ERC aims to: support the best of the best in Europe across all fields of science, scholarship and engineering; promote wholly investigator-driven, or 'bottom-up' frontier research; encourage the work of the established and next generation of independent top research leaders in Europe; reward innovative proposals by placing emphasis on the quality of the idea rather than the research area; and raise the status and visibility of European frontier research and the very best researchers of today and tomorrow.
Sparks
Sparks aims to improve the quality of life for children and families affected by serious illness or disability today, whilst seeking ways to better diagnose, treat and prevent these conditions in the future. They fund research across the wholes spectrum of paediatric medicine from some of the most common conditions, including childhood arthritis, meningitis, cerebral palsy and spina bifida to some of the rarest conditions. The medical breakthroughs they make possible make a difference not only across the UK but for thousands of children and families around the world.
Wellcome
Wellcome exists to improve health for everyone by helping great ideas to thrive. Wellcome is a global charitable foundation, both politically and financially independent, supporting scientists and researchers to take on big problems, fuel imaginations, and spark debate. Wellcome remains true to the vision and values of their founder, Sir Henry Wellcome, a medical entrepreneur, collector and philanthropist. The work of Wellcome today reflects the amazing breadth of Henry's interests, and his belief that science and research expand knowledge by testing and investigating ideas. Wellcome funding supports over 14,000 people in more than 70 countries. In the next five years, they aim to spend up to £5 billion helping thousands of curious, passionate people all over the world explore ideas in science, population health, medical innovation, the humanities and social sciences and public engagement.


